An article from Cancer Treatment Centers of America Website:
Receiving a diagnosis of pancreatic cancer is considered a grave diagnosis. Many patients having Pancreatic cancer don’t present for diagnosis until in later stages of the disease, mainly because there are usually few symptoms affecting the patient.
Development of Pancreatic Cancer
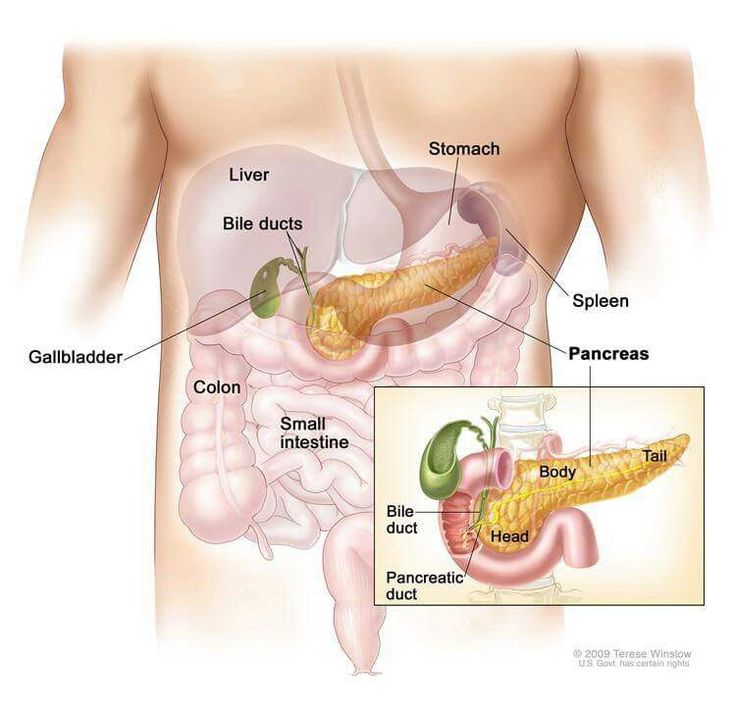
Pancreatic cancer develops in the tissues of the pancreas, an organ located behind the lower portion of the stomach. The pancreas aids in digestion, metabolism and insulin production. Cancer may develop in either the exocrine glands or the endocrine glands of the pancreas. About 95 percent of pancreatic cancers begin in the exocrine glands (the cells that produce the enzymes or “digestive juices” that help break down proteins, fats and starches).
Pancreatic cancer affects the body’s ability to digest and absorb vital nutrients from food. This may cause nausea, taste changes, weight loss, fatigue, decreased appetite, fullness, pain, gas, diarrhea and constipation. Over time, these symptoms may put patients at risk for malnutrition.
Having good nutrition is so important during treatment for pancreatic cancer, no matter the stage of the diagnosis.
Because part of the pancreas is removed during surgery, the part that remains after surgery may not be able to produce enough enzymes to properly aid with the digestion of food, and patients may not be able to digest or absorb the fat from the food they eat. When undigested fat remains in the stool, it causes diarrhea and poor nutrition. Patients may also experience bloating, excessive gas production and abdominal cramping. Consequently, the goal for these patients is to eliminate or reduce diarrhea, restore adequate nutrition, prevent weight loss and manage bloating, cramping and gas.
Patients who have had a Whipple surgery are more likely than those who have had a distal pancreatectomy (another type of pancreatic surgery) to have insufficient enzyme production.
General recommendations following pancreatic surgery
- Take the prescribed amount of pancreatic enzyme replacement products with all meals and snacks.
- Gradually start adding solid foods. The timing of this varies from individual to individual.
- Avoid high-fat, greasy or fried foods.
- Eat 6-8 small meals and snacks daily to prevent feeling overly full. Small meals are easier to digest. Space meals 2-3 hours apart.
- Drink at least 6-12 cups of fluids each day. Lack of fluids may lead to fatigue, light-headedness and nausea.
- Take small sips of liquids with meals. Drinking too much fluid at mealtime may cause the patient to feel full quicker or increase nausea. Drink liquids an hour before or after eating to avoid feeling full.
- Drink beverages that contain calories, nutrients and protein, such as juices, smoothies or nutritional supplement drinks. It is acceptable to drink small amounts of these at mealtimes or to use nutritional supplement drinks or protein smoothies as meal/snack replacements.
- Avoid alcoholic beverages.
- If the patient is nauseated and has an empty stomach, small bites of dry foods are often better tolerated than liquids.
- Avoid eating concentrated refined/simple carbohydrates if symptoms of glucose intolerance or dumping are present. Glucose intolerance symptoms include increased thirst, frequent urination, blurry vision and fatigue. Dumping symptoms usually occur within 2 hours after eating and include flushed skin, dizziness/lightheadedness, weakness, abdominal pain, nausea, vomiting and diarrhea.
- Discuss with your doctor or dietitian the use of a multivitamin or individual vitamin supplements. Calcium and the fat-soluble vitamins A, D, E and K may be necessary if malabsorption-induced diarrhea is present. Ask a healthcare professional for a proper dosage of individual vitamin supplements.
- If anemia occurs, ask the doctor whether iron supplements or injections of vitamin B12 may be helpful.